I had a LONG clinic yesterday afternoon–walked out the door at 6pm to make it to another meeting accross town, and left some things undone.
I had a LONG clinic yesterday afternoon–walked out the door at 6pm to make it to another meeting accross town, and left some things undone.
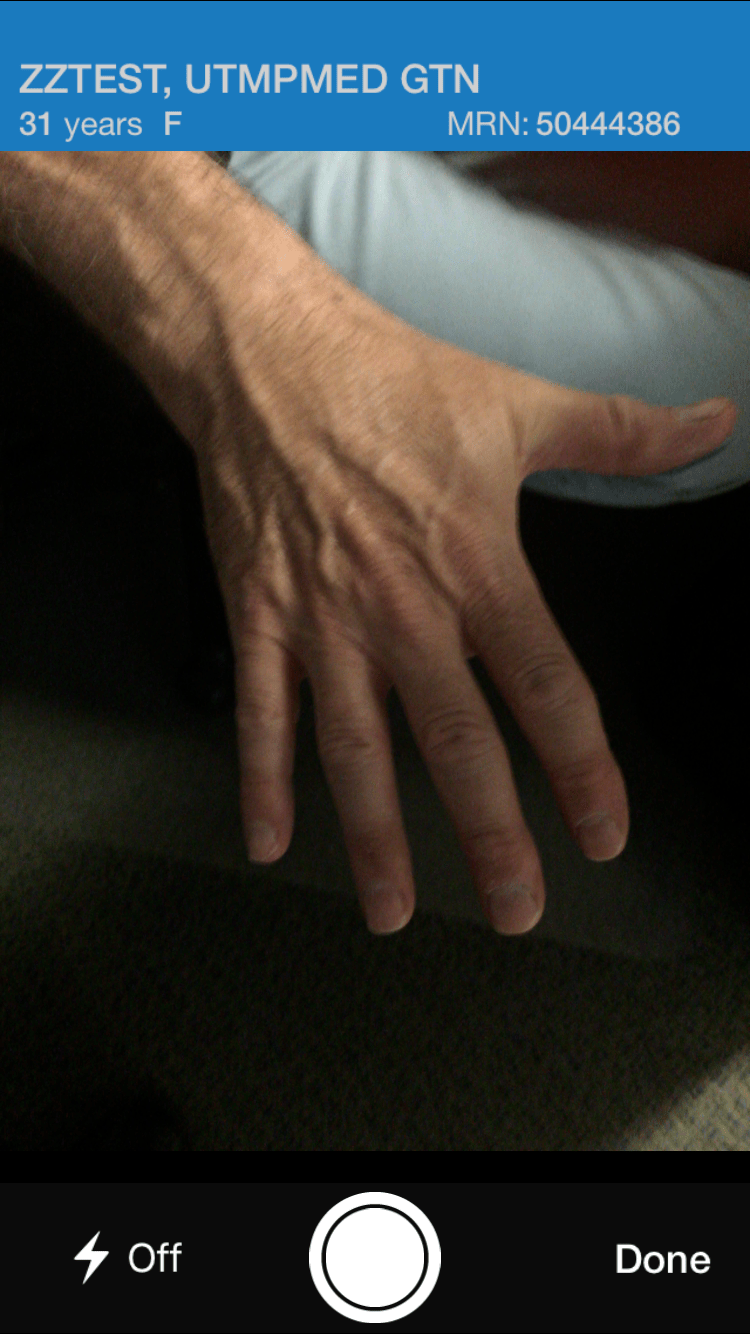
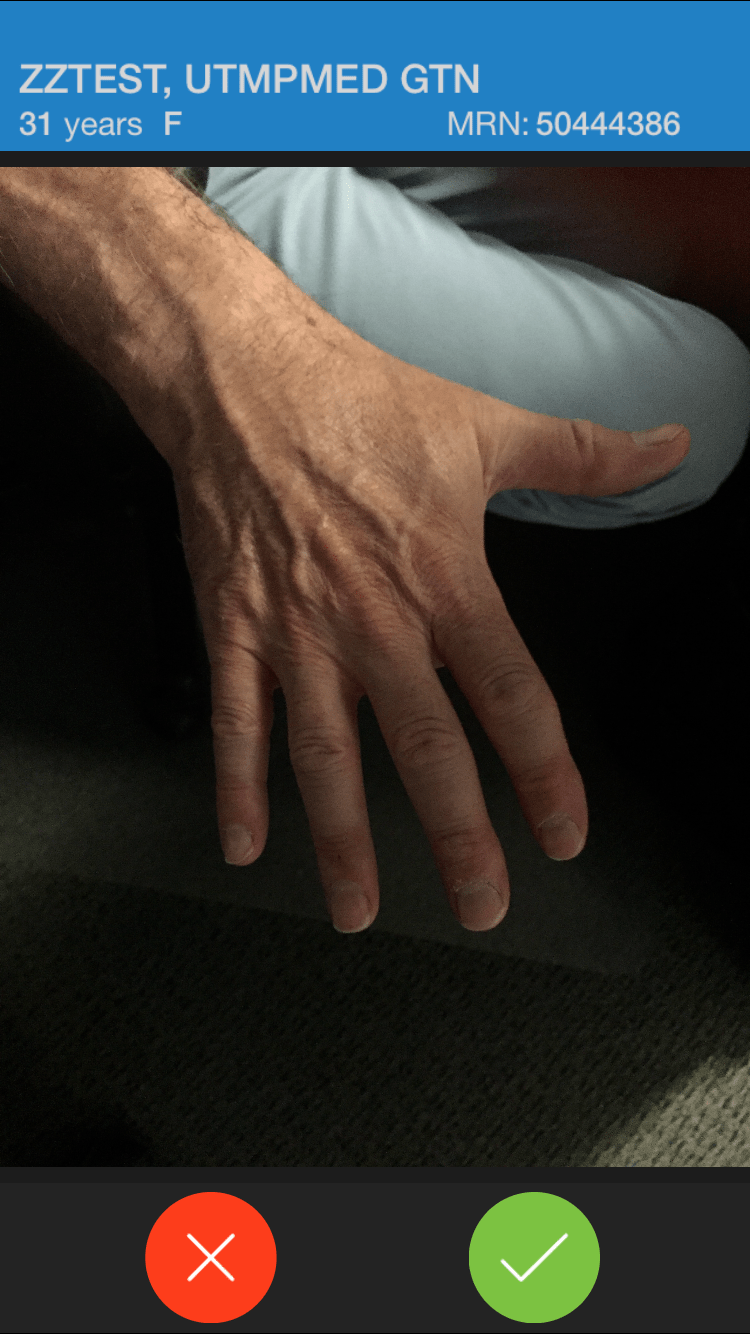
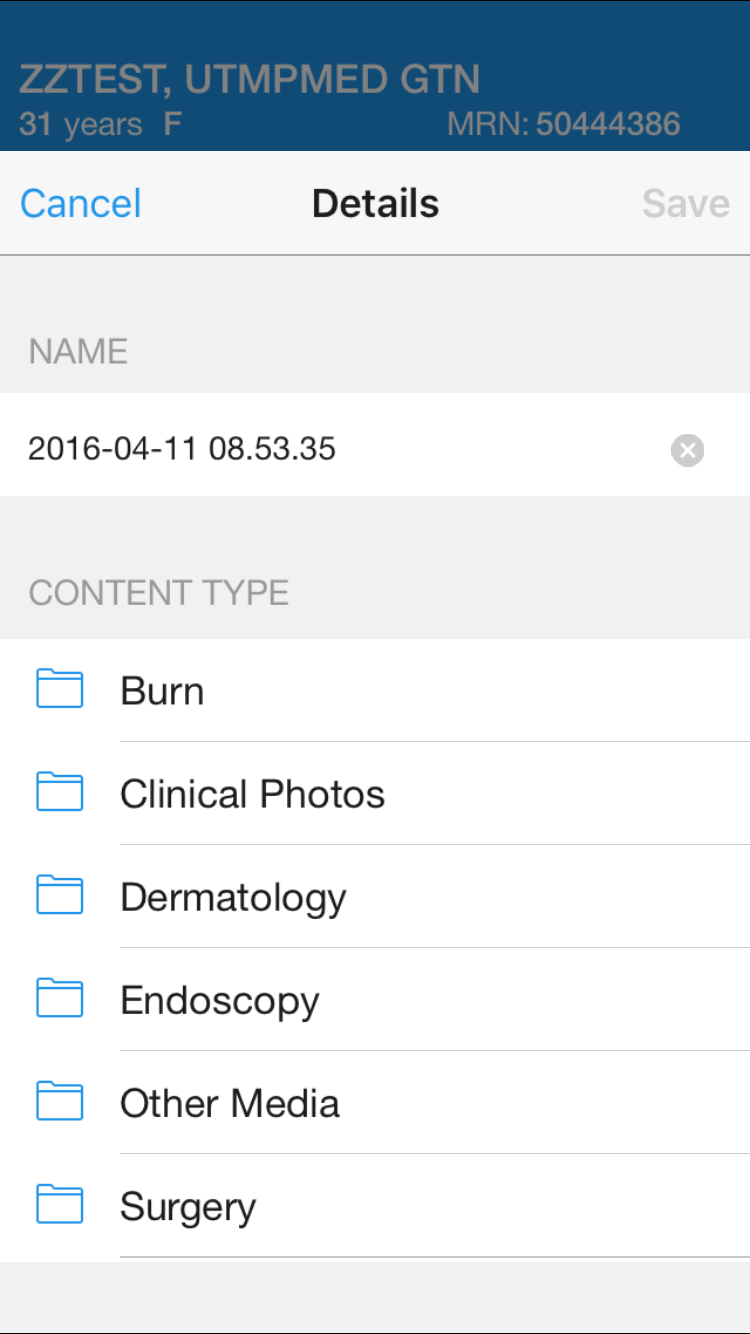
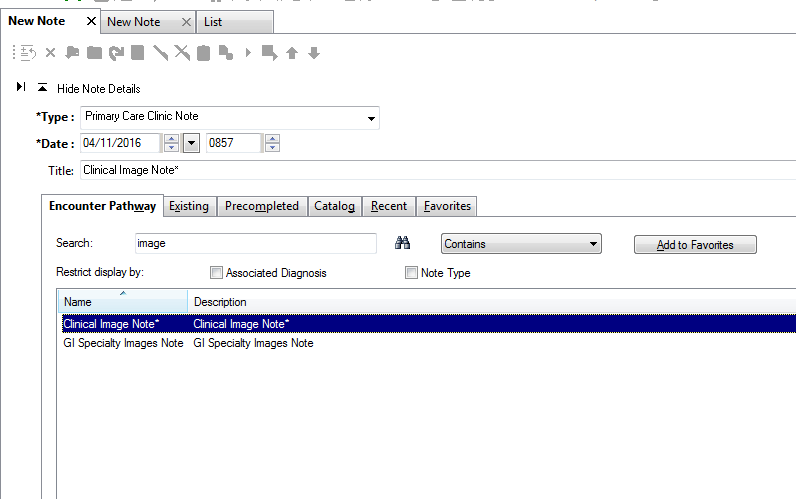
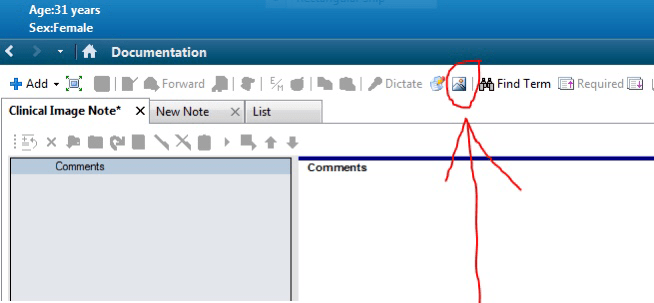
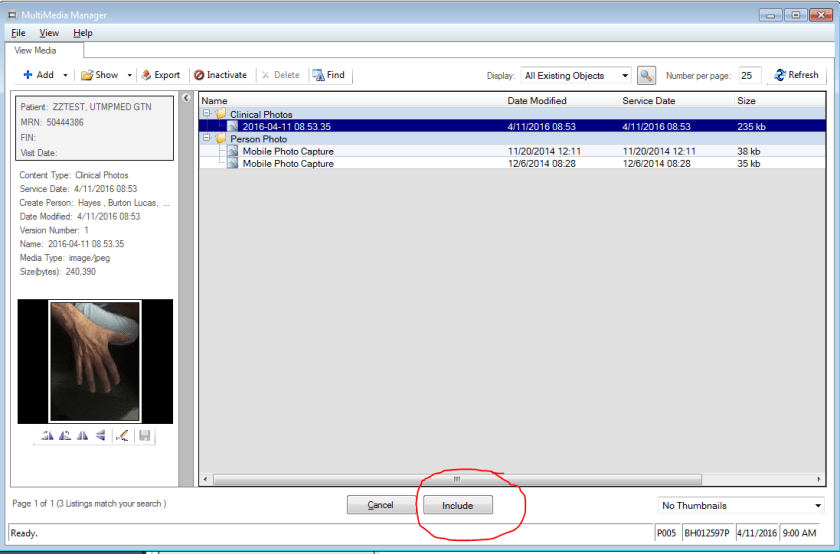
Today I’m on a long flight. Thanks to the suite of Powerchart Touch apps (Powerchart Touch, Message Center, Camera Capture) once I hooked up to wifi, I was able to catch up on lab review, send results directly to patients via the Patient Portal, and finish my charts. Yes, I needed to buy WiFi on the flight (I usually do anyway on long flights) and I have to tilt my iPad screen just a little to keep prying eyes away from patient information. But still, this is pretty cool stuff, folks. I would encourage to try the apps out. Powerchart Touch is available for iOS in the AppStore. You will need an access code to use it the first time. You can obtain an access code via the Helpdesk (516-3111). Message Center is available for iOS and coming soon to Android. Camera Capture is available for both iOS and Android. You only need to use the access code once. Once your device is enrolled, you can use any of the Powerchart Touch apps.
This is a really bumpy flight, but charting was SMOOOTH!